Table of Contents
Introduction
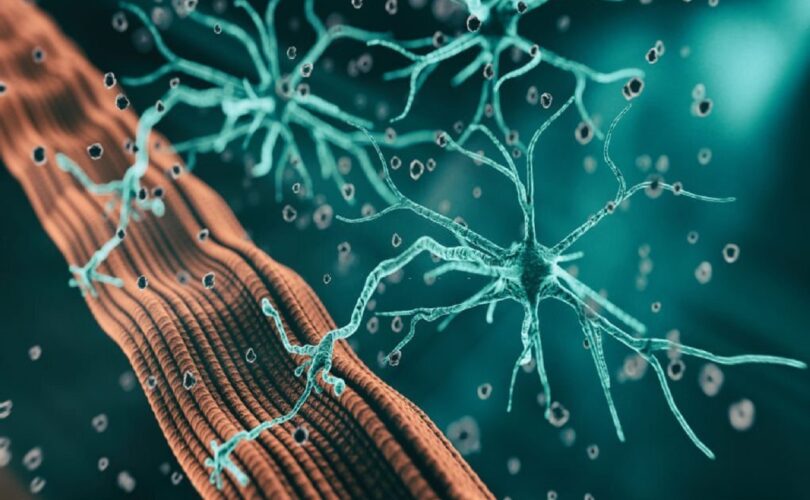
Welcome to an overview of Neuromuscular Blockers! These drugs are commonly used in medical settings, and today we’ll be diving into the pharmacology and clinical uses of these curious substances. Neuromuscular Blockers are drugs that cause paralysis of skeletal muscles. They are used for various reasons in medical settings, such as facilitating intubation during surgery, reducing muscle contractions during diagnostic tests, and aiding mechanical ventilation during critical care. But how do they work?
Neuromuscular Blockers function by binding to acetylcholine receptors at the neuromuscular junction, blocking the neurotransmitter’s action. This causes muscle relaxation and, in higher doses, paralysis. Now that we’ve established what Neuromuscular Blockers are and their mechanism of action let’s dive into the different types of these drugs, their onset, duration, and administration – so stay tuned!
Pharmacology of Neuromuscular Blockers
Neuromuscular blockers are drugs that are administered to temporarily paralyze skeletal muscles by blocking the transmission of nerve impulses. This effect is achieved by interfering with the action of acetylcholine at the neuromuscular junction. Neuromuscular blockers are used in medical settings to facilitate intubation, ventilation, and surgical procedures.
The structure of neuromuscular blockers is such that they can either be depolarizing or non-depolarizing agents. The mechanism of action for the two groups of drugs is different. Depolarizing neuromuscular blockers, for instance, mimic the action of acetylcholine, leading to sustained depolarization of muscle fibers. In contrast, non-depolarizing neuromuscular blockers bind to the α-subunit of nicotinic receptors, thereby preventing the conformational change required for the opening of the ion channel.
There are different types of neuromuscular blockers, with the most common ones being atracurium, vecuronium, and rocuronium. These drugs differ in their onset, duration, and speed of elimination. For instance, atracurium has a rapid onset and is associated with histamine release, while vecuronium has a longer duration of action and is metabolized by the liver. Similarly, rocuronium has intermediate duration of action and does not cause histamine release, making it a suitable choice in patients with cardiovascular instability.
The onset of neuromuscular blockers is dependent on factors such as their physicochemical properties, dosage, and mode of administration. The duration of action, on the other hand, is influenced by factors such as hepatic and renal function, drug interactions, and patient age. Reversal agents such as neostigmine and sugammadex can be used to antagonize the effects of neuromuscular blockers, thereby permitting the return of muscle strength.
In conclusion, Neuromuscular blockers play an essential role in clinical practice, especially in patients requiring mechanical ventilation and surgical procedures. Understanding the pharmacology of these drugs is crucial in ensuring their safe and efficacious use. Different neuromuscular blockers have varying physicochemical properties, onset, duration, and reversal agents. Thus, healthcare professionals should be familiar with these characteristics to make informed clinical decisions.
Administration of Neuromuscular Blockers
Let’s talk about the administration of neuromuscular blockers. We’ve already covered what they do and why they’re used, but how are they given? First, let’s talk dosage and route of administration. Neuromuscular blockers are typically given intravenously, which means they’re injected directly into a vein.
The dose varies depending on the specific drug used, the patient’s weight, and the desired level of neuromuscular blockade. It’s important to get the dosage right because too little won’t be effective, but too much could lead to complications. That brings us to our next point. Monitoring during administration is crucial. Patients receiving neuromuscular blockers need to be carefully monitored to ensure they remain sedated and still, but also to watch for any potential issues.
This includes monitoring for respiratory distress and making sure the patient remains stable throughout the procedure. Of course, like any medication, there are potential complications associated with the use of neuromuscular blockers. Some patients may have an allergic reaction, and there is always the risk of infection at the injection site. Additionally, overuse of neuromuscular blockers can cause prolonged paralysis or even muscle weakness after the medication wears off.
Overall, administering neuromuscular blockers is a delicate process that requires close attention and monitoring. It’s not something to be taken lightly, but in the right hands, it can be a powerful tool in the medical setting.
Clinical Applications
When it comes to clinical applications of neuromuscular blockers, there are a few key areas where they are commonly used. One such area is general anesthesia. Neuromuscular blockers can be used in conjunction with other anesthesia medications to help achieve a safe and effective level of muscle relaxation during surgery. Surgery, in general, is another area where neuromuscular blockers can be useful.
By relaxing certain muscles, these drugs can facilitate surgical procedures and improve surgical outcomes. In addition to anesthesia and surgery, neuromuscular blockers are also used in diagnostic testing. By relaxing certain muscles, these drugs can help doctors get a better look at specific areas of the body during imaging tests such as X-rays and CT scans.
For patients who require mechanical ventilation, neuromuscular blockers can be used to help manage their breathing. By relaxing the muscles responsible for breathing, patients can benefit from more effective ventilation and improved oxygenation.
Finally, neuromuscular blockers can be used in critical care settings to manage conditions such as acute respiratory distress syndrome and status asthmaticus. Overall, the clinical applications of neuromuscular blockers are varied and diverse, and these drugs can be an important tool in the medical toolkit.
Conclusion
Pharmacology of Neuromuscular Blockers is an educationally beneficial concept. To sum it up, Neuromuscular blockers are drugs that relax muscle tone and produce skeletal muscle paralysis by interfering with neurotransmission at the neuromuscular junction. Administering these drugs can help in various medical settings, including surgery, mechanical ventilation, and critical care.
Although they come with potential complications, they are widely used. Future research should focus on developing newer, shorter-acting, more selective, and, importantly, safer Neuromuscular Blockers. Overall, Neuromuscular Blockers continue to play an essential role in modern medicine, and we hope that this blog has helped you understand just how beneficial these drugs can be.
Read This Also: Histamine and Histamines Pharmacology