Table of Contents
Chapter 5 Haemopoietic System
LONG ESSAYS (10Marks)
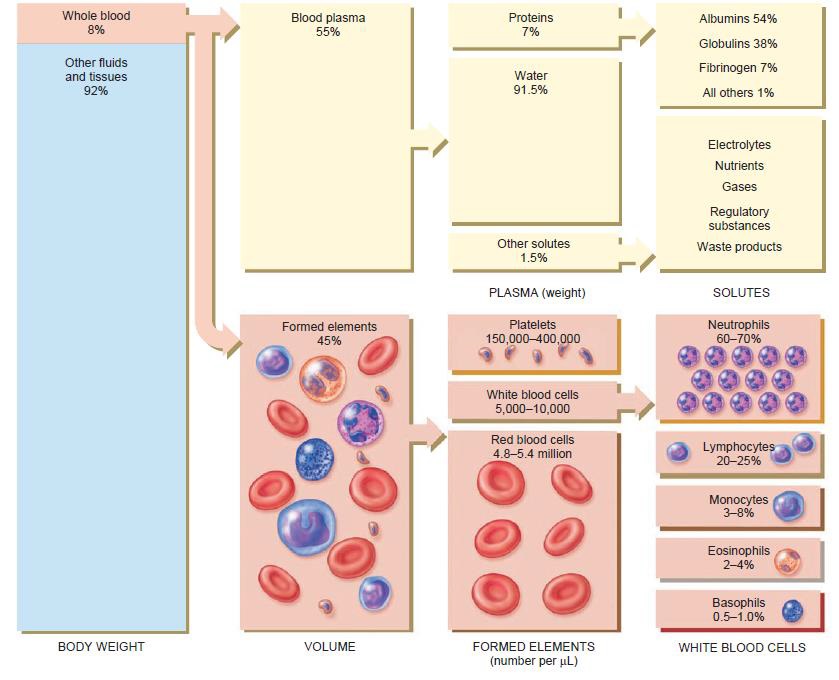
1. Describe the constituents of blood and their functions.
Answer: PLASMA
When formed elements are removed from the blood, a straw-colored liquid called blood plasma is left.
| OTHER SOLUTES (1.5%)
ELECTROLYTES |
Inorganic salts. Positively charges ions(cations) include Na+,K+,Ca+,Mg2+;
Negatively charged ions(anions) include Cl-,HPO42-,SO42-,HCO3-. Help maintain osmotic pressure and plays essential roles in the function of cells. |
| NUTRIENTS | Products of digestion pass into the blood for distribution to all body cells. Includes amino acids(from proteins), glucose(from carbohydrates), fatty acids and glycerol(from triglycerides), vitamins and minerals. |
| GASES | Oxygen, Carbon dioxide, and Nitrogen. More O2 is associated with hemoglobin inside red blood cells; more CO2 is dissolved in plasma. N2 is present but has no known functions in the body. |
| REGULATORY SUBSTANCES | Enzymes produce by body cells, catalyze chemical reactions. Hormones, produced by endocrine glands, regulate metabolism, growth, and development. Vitamins are cofactors for enzymatic reactions. |
| WASTE PRODUCTS | Most are breakdown products of protein metabolism and are carried by the blood to organs of excretion. Include urea, uric acid, creatine, creatinine, bilirubin and ammonia. |
| WATER (91.5%) | The liquid portion of blood. Acts as the solvent and suspending medium for components of blood; absorbs, transports, and releases heat. |
| PLASMA PROTEIN (7.0%) | Exert colloid osmotic pressure, which helps maintain water balance between blood and tissues and regulates blood volume. |
| ALBUMIN | Smallest and most numerous blood plasma proteins; produced by the liver. Transports proteins for several steroid hormones and for fatty acids. |
| GLOBULINS | Produces by liver and plasma cells, which develop from B lymphocytes. Antibodies help attack viruses and bacteria. Alpha and beta globulins transport iron, lipids, and fat-soluble vitamin. |
| FIBRINOGEN | Produces by the liver. Plays an essential role in blood clotting. |
| FORMED ELEMENTS | FUNCTIONS |
| Red Blood Cells(RBCs) or Erythrocytes | Hemoglobin within RBCs transports most of the oxygen and part of carbon dioxide in the blood. |
| White Blood Cells(WBCs) or Leukocytes | Combat pathogen and other foreign substances that enter the body. |
| Granular Leukocytes
Neutrophiles |
Phagocytosis. Destruction of bacteria with lysozymes, defensins and strong oxidants, such as superoxide anion, hydrogen peroxide, and hypochlorite anion. |
| Eosinophils | Eliminates parasites, such as worms which are too big to be phagocytosed; phagocytes antigen-antibody complexes & combat the effects of histamine in allergic reactions. |
| Basophils | Liberate heparin, histamine and serotonin in allergic reactions that intensify the overall inflammatory response. |
| Agranular Leukocytes
Lymphocytes(T cells, B cells & natural killer cells) |
Medium immune response, including antigen-antibody reactions. B cells develop into plasma cells, which secrete antibodies, T cells attack invading viruses, cancer cells, and transplanted tissue cells. Natural killer calls attach a wide variety of infectious microbes and certain spontaneously arising tumor cells. |
| Monocytes | Acts on the hypothalamus, causing the rise in body temperature with microbial infections; stimulates the production of some globulins by the liver; enhances the production of activated T-lymphocytes; Phagocytosis. |
| Platelets(Thrombocytes) | Form platelet plug in homeostasis; release chemicals that promote vascular spasm and blood clotting. |
Blood is a specialized body fluid. It has four main components: plasma, red blood cells, white blood cells, and platelets. Blood has many different functions, including transporting oxygen and nutrients to the lungs and tissues.
2.Mention coagulation factors and write the mechanism of blood coagulation
Answer: Coagulation Factors
• I Fibrinogen
• II Prothrombin
• III Tissue factor (thromboplastin)
• IV Calcium (Ca2+)
• V Labile factor, proaccelerin, Ac-globulin
• VII Stable factor, proconvertin
• VIII Antihaemophilic globulin (AHG), antihaemophilic factor A
• IX Christmas factor, plasma thromboplastin component (PTA), antihaemophilic factor B
• X Stuart Prower factor
• XI Plasma thromboplastin antecedent (PTA), antihaemophilic factor C
• XII Hageman factor
• XIII Fibrin stabilizing factor
• Vitamin K is essential for the synthesis of factors II, VII, IX, and X.
Stages of blood coagulation
This is a complex process that also involves a positive feedback system. The factors involved are listed above. These clotting factors activate each other in a specific order, eventually resulting in the formation of a prothrombin activator, which is the first step in the final common pathway. Prothrombin activates the enzyme thrombin, which converts inactive fibrinogen to insoluble threads of fibrin. As clotting proceeds, the platelet plug is progressively stabilized by increasing amounts of fibrin laid down in a three-dimensional meshwork within it. The maturing blood clot traps blood cells and other plasma proteins including plasminogen (which will eventually destroy the clot) and is much stronger than the rapidly formed platelet plug.
 The final common pathway can be initiated by two processes that often occur together: the extrinsic and intrinsic pathways. The extrinsic pathway is activated rapidly (within seconds) following tissue damage. Damaged tissue releases a complex of chemicals called thromboplastin or tissue factor, which initiates coagulation. The intrinsic pathway is slower (3–6 minutes) and is triggered when blood comes into contact with the damaged blood vessel lining (endothelium). After a time the clot shrinks (retracts) because the platelets contract, squeezing out the serum, a clear sticky fluid that consists of plasma from which clotting factors have been removed. Clot shrinkage pulls the edges of the damaged vessel together, reducing blood loss and closing off the hole in the vessel wall.
The final common pathway can be initiated by two processes that often occur together: the extrinsic and intrinsic pathways. The extrinsic pathway is activated rapidly (within seconds) following tissue damage. Damaged tissue releases a complex of chemicals called thromboplastin or tissue factor, which initiates coagulation. The intrinsic pathway is slower (3–6 minutes) and is triggered when blood comes into contact with the damaged blood vessel lining (endothelium). After a time the clot shrinks (retracts) because the platelets contract, squeezing out the serum, a clear sticky fluid that consists of plasma from which clotting factors have been removed. Clot shrinkage pulls the edges of the damaged vessel together, reducing blood loss and closing off the hole in the vessel wall.
3. Describe the process of Erythropoiesis and factors required or influencing erythropoiesis.
Answer: Erythropoiesis the production of RBCs, starts in the red bone marrow with a precursor cell called a proerythroblast. The proerythroblast divides several times, producing cells that begin to synthesize hemoglobin. Ultimately, a cell near the end of the development sequence ejects its nucleus and becomes a reticulocyte. Loss of the nucleus causes the center of the cell to indent, producing the red blood cell’s distinctive biconcave shape.
 Reticulocytes retain some mitochondria, ribosomes, and endoplasmic reticulum. They pass from the red bone marrow into the bloodstream by squeezing between the endothelial cells of blood capillaries. Reticulocytes develop into mature red blood cells within 1 to 2 days after their release from red bone marrow. Normally, erythropoiesis and red blood cell destruction proceed at roughly the same pace. If the oxygen-carrying capacity of the blood falls because erythropoiesis is not keeping up with RBC destruction, a negative feedback system steps up RBC production. The controlled condition is the amount of oxygen delivered to body tissues. Cellular oxygen deficiency, called hypoxia, may occur if too little oxygen enters the blood. For example, the lower oxygen content of air at high altitudes reduces the amount of oxygen in the blood. Oxygen delivery may also fall due to anemia, which has many causes: Lack of iron, lack of certain amino acids, and lack of vitamin B12 are but a few. Circulatory problems that reduce blood flow to tissues may also reduce oxygen delivery. Whatever the cause, hypoxia stimulates the kidneys to step up the release of erythropoietin, which speeds the development of proerythroblasts into reticulocytes in the red bone marrow. As the number of circulating RBCs increases, more oxygen can be delivered to body tissues.
Reticulocytes retain some mitochondria, ribosomes, and endoplasmic reticulum. They pass from the red bone marrow into the bloodstream by squeezing between the endothelial cells of blood capillaries. Reticulocytes develop into mature red blood cells within 1 to 2 days after their release from red bone marrow. Normally, erythropoiesis and red blood cell destruction proceed at roughly the same pace. If the oxygen-carrying capacity of the blood falls because erythropoiesis is not keeping up with RBC destruction, a negative feedback system steps up RBC production. The controlled condition is the amount of oxygen delivered to body tissues. Cellular oxygen deficiency, called hypoxia, may occur if too little oxygen enters the blood. For example, the lower oxygen content of air at high altitudes reduces the amount of oxygen in the blood. Oxygen delivery may also fall due to anemia, which has many causes: Lack of iron, lack of certain amino acids, and lack of vitamin B12 are but a few. Circulatory problems that reduce blood flow to tissues may also reduce oxygen delivery. Whatever the cause, hypoxia stimulates the kidneys to step up the release of erythropoietin, which speeds the development of proerythroblasts into reticulocytes in the red bone marrow. As the number of circulating RBCs increases, more oxygen can be delivered to body tissues.
SHORT ESSAYS (5M)
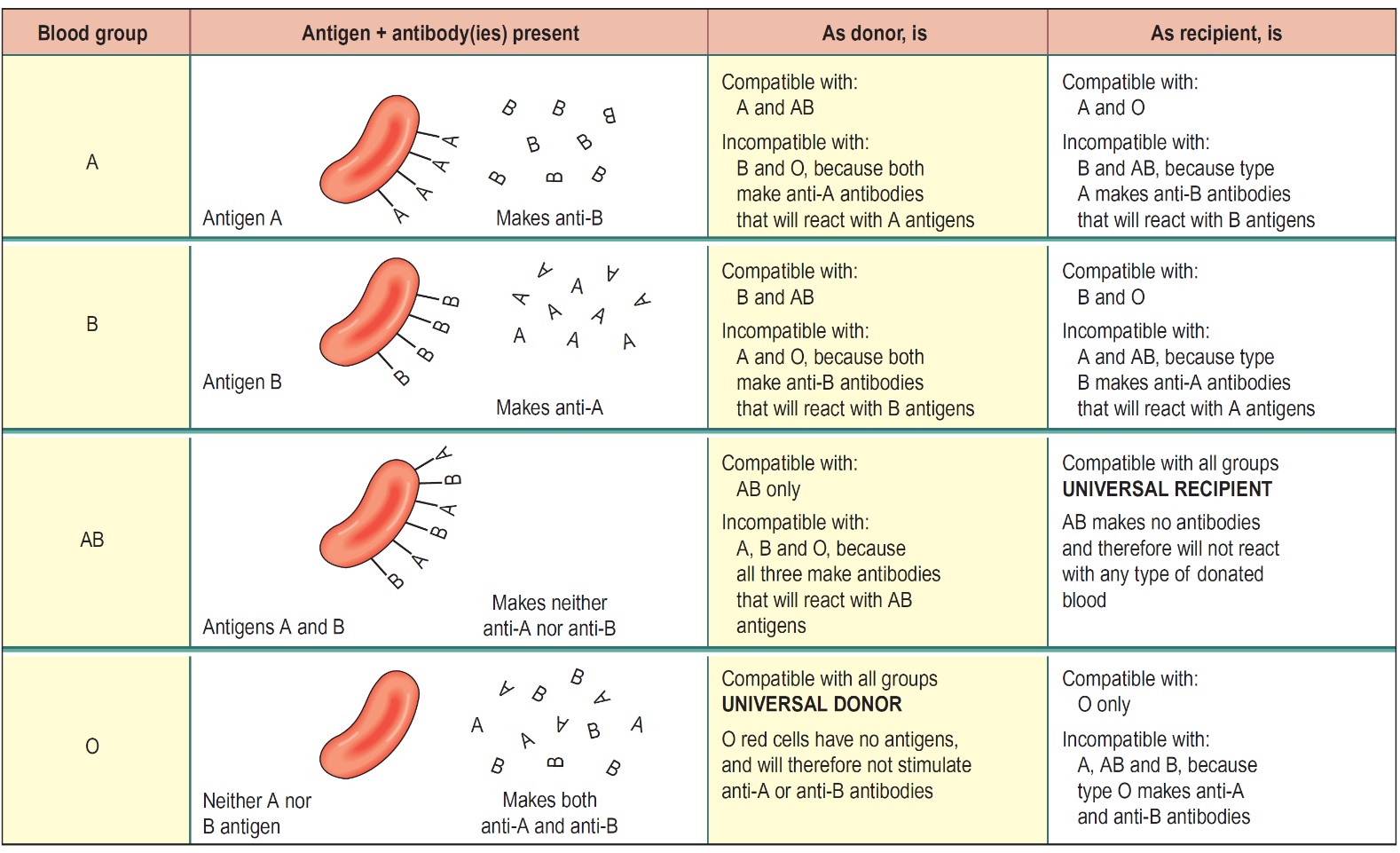
1. Describe the ABO system of blood grouping.
Answer:
2. Describe the structure and functions of platelets.
Answer:
These are very small discs, 2–4 μm in diameter, derived from the cytoplasm of megakaryocytes in the red bone marrow. Although they have no nucleus, their cytoplasm is packed with granules containing a variety of substances that promote blood clotting, which causes hemostasis (cessation of bleeding). The normal blood platelet count is between 200 × 109/L and 350 × 109/L (200 000–350 000/mm3). The mechanisms that regulate platelet numbers are not fully understood, but the hormone thrombopoietin from the liver stimulates platelet production. The life span of platelets is between 8 and 11 days and those not used in hemostasis are destroyed by macrophages, mainly in the spleen. About a third of platelets are stored within the spleen rather than in the circulation; this is an emergency store that can be released as required to control excessive bleeding.
Function-Form platelet plug in hemostasis; release chemicals that promote vascular spasm and blood clotting.
3. Write any eight functions of blood.
Answer: Blood has three main functions: transport, protection, and regulation.
Transport
Blood transports the following substances:
• Gases, namely oxygen (O2) and carbon dioxide (CO2), between the lungs and rest of the body
• Nutrients from the digestive tract and storage sites to the rest of the body
• Waste products to be detoxified or removed by the liver and kidneys
• Hormones from the glands in which they are produced to their target cells
• Heat to the skin so as to help regulate body temperature.
Protection
Blood has several roles in inflammation:
• Leukocytes, or white blood cells, destroy invading microorganisms and cancer cells
• Antibodies and other proteins destroy pathogenic substances
• Platelet factors initiate blood clotting and help minimize blood loss.
Regulation
Blood helps regulate:
• pH by interacting with acids and bases
• Water balance by transferring water to and from tissues
4. What is anemia? Explain its types
Answer: Anaemia is the inability of the blood to carry enough oxygen to meet body needs. Usually, this is because there are low levels of hemoglobin in the blood, but sometimes it is due to the production of faulty hemoglobin.
• Iron deficiency anemia. This is the most common type of anemia worldwide. Iron deficiency anemia is caused by a shortage of iron in your body. Your bone marrow needs iron to make hemoglobin. Without adequate iron, your body can’t produce enough hemoglobin for red blood cells.
• Vitamin deficiency anemia. In addition to iron, your body needs folate and vitamin B-12 to produce enough healthy red blood cells. A diet lacking in these and other key nutrients can cause decreased red blood cell production.
• Anemia of chronic disease. Certain diseases — such as cancer, HIV/AIDS, rheumatoid arthritis, kidney disease, Crohn’s disease, and other chronic inflammatory diseases — can interfere with the production of red blood cells.
• Aplastic anemia. This rare, life-threatening anemia occurs when your body doesn’t produce enough red blood cells. Causes of aplastic anemia include infections, certain medicines, autoimmune diseases, and exposure to toxic chemicals.
• Anemias associated with bone marrow disease. A variety of diseases, such as leukemia and myelofibrosis, can cause anemia by affecting blood production in your bone marrow. The effects of these types of cancer and cancer-like disorders vary from mild to life-threatening.
• Hemolytic anemias. This group of anemias develops when red blood cells are destroyed faster than bone marrow can replace them. Certain blood diseases increase red blood cell destruction. You can inherit a hemolytic anemia, or you can develop it later in life.
• Sickle cell anemia. This inherited and sometimes serious condition is inherited hemolytic anemia. It’s caused by a defective form of hemoglobin that forces red blood cells to assume an abnormal crescent (sickle) shape. These irregular blood cells die prematurely, resulting in a chronic shortage of red blood cells.
• Other anemias. There are several other forms of anemia, such as thalassemia and malarial anemia.
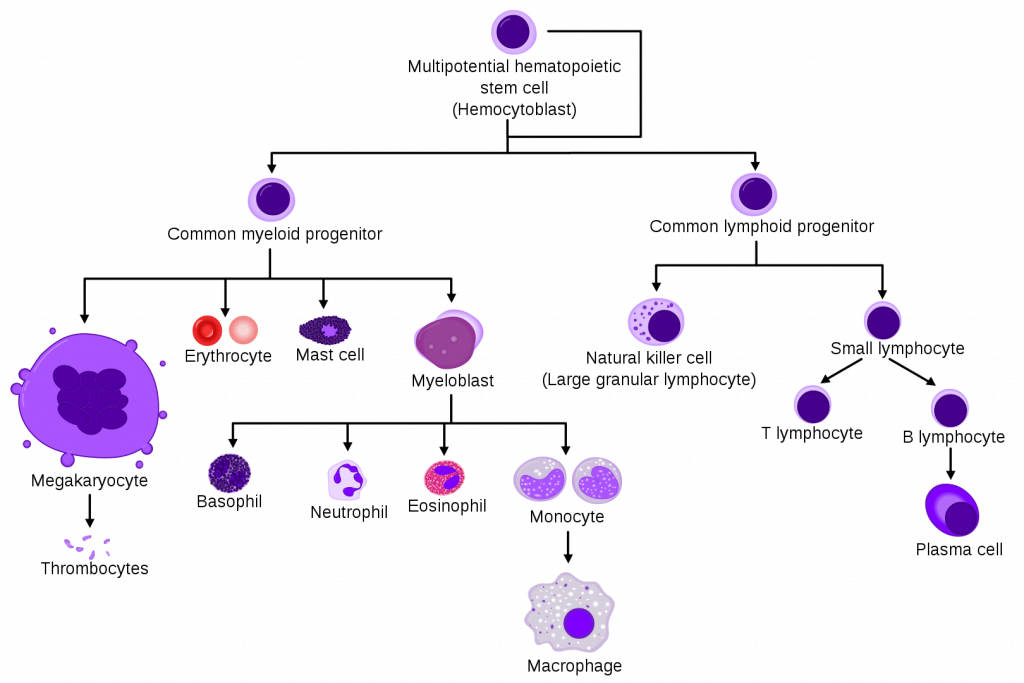
5. Classify leucocytes. Mention its functions.
Answer:
| White Blood Cells(WBCs) or Leukocytes | Combat pathogen and other foreign substances that enter the body. |
| Granular Leukocytes
Neutrophiles |
Phagocytosis. Destruction of bacteria with lysozymes, defensins and strong oxidants, such as superoxide anion, hydrogen peroxide, and hypochlorite anion. |
| Eosinophils | Eliminates parasites, such as worms which are too big to be phagocytosed; phagocytes antigen-antibody complexes & combat the effects of histamine in allergic reactions. |
| Basophils | Liberate heparin, histamine and serotonin in allergic reactions that intensify the overall inflammatory response. |
| Agranular Leukocytes
Lymphocytes(T cells, B cells & natural killer cells) |
Medium immune response, including antigen-antibody reactions. B cells develop into plasma cells, which secrete antibodies, T cells attack invading viruses, cancer cells, and transplanted tissue cells. Natural killer calls attach a wide variety of infectious microbes and certain spontaneously arising tumor cells. |
| Monocytes | Acts on the hypothalamus, causing the rise in body temperature with microbial infections; stimulates the production of some globulins by the liver; enhances the production of activated T-lymphocytes; Phagocytosis. |
6. Explain the factors influencing blood coagulation.
Answer: coagulation factors
 • I Fibrinogen
• I Fibrinogen
• II Prothrombin
• III Tissue factor (thromboplastin)
• IV Calcium (Ca2+)
• V Labile factor, proaccelerin, Ac-globulin
• VII Stable factor, proconvertin
• VIII Antihaemophilic globulin (AHG), antihaemophilic factor A
• IX Christmas factor, plasma thromboplastin component (PTA), antihaemophilic factor B
• X Stuart Prower factor
• XI Plasma thromboplastin antecedent (PTA), antihaemophilic factor C
• XII Hageman factor
• XIII Fibrin stabilizing factor
• Vitamin K is essential for the synthesis of factors II, VII, IX, and X.
7. What is the basis for the Rh system? Write a note on the hemolytic disease of the newborn (erythroblastosis fetalis).
Answer:
The red blood cell membrane antigen important here is the Rhesus (Rh) antigen or Rhesus factor. About 85% of people have this antigen; they are Rhesus positive (Rh+) and do not, therefore, make anti-Rhesus antibodies. The remaining 15% have no Rhesus antigen (they are Rhesus negative or Rh−). Rh− individuals are capable of making anti-Rhesus antibodies, but are stimulated to do so only in certain circumstances, e.g. in pregnancy, or as the result of an incompatible blood transfusion.
Erythroblastosis fetalis
In this disorder, the mother’s immune system makes antibodies to the baby’s red blood cells, causing the destruction of fetal erythrocytes. The antigen system involved is usually (but not always) the Rhesus (Rh) antigen. An Rh− mother carries no Rh antigen on her red blood cells, but she has the capacity to produce anti-Rh antibodies. If she conceives a child fathered by a Rh+ man, and the baby inherits the Rh antigen from him, the baby may also be Rh+, i.e. different from the mother. During pregnancy, the placenta protects the baby from the mother’s immune system, but at delivery, a few fetal red blood cells may enter the maternal circulation. Because they carry an antigen (the Rh antigen) foreign to the mother, her immune system will be stimulated to produce neutralising antibodies to it. The red cells of second and subsequent Rh+ babies are attacked by these maternal antibodies, which can cross the placenta and enter the fetal circulation. In the most severe cases, the baby dies in the womb from profound anemia. In less serious circumstances, the baby is born with some degree of anemia, which is corrected with blood transfusions.
8. Describe the constituents of plasma and their functions?
Answer:
| OTHER SOLUTES (1.5%)
ELECTROLYTES |
Inorganic salts. Positively charges ions(cations) include Na+,K+,Ca+,Mg2+;
Negatively charged ions(anions) include Cl-,HPO42-,SO42-,HCO3-. Help maintain osmotic pressure and plays essential roles in the function of cells. |
|
| NUTRIENTS | Products of digestion pass into the blood for distribution to all body cells. Includes amino acids(from proteins), glucose(from carbohydrates), fatty acids and glycerol(from triglycerides), vitamins and minerals. | |
| GASES | Oxygen, Carbon dioxide, and Nitrogen. More O2 is associated with hemoglobin inside red blood cells; more CO2 is dissolved in plasma. N2 is present but has no known functions in the body. | |
| REGULATORY SUBSTANCES | Enzymes produce by body cells, catalyze chemical reactions. Hormones, produced by endocrine glands, regulate metabolism, growth, and development. Vitamins are cofactors for enzymatic reactions. | |
| WASTE PRODUCTS | Most are breakdown products of protein metabolism and are carried by the blood to organs of excretion. Include urea, uric acid, creatine, creatinine, bilirubin and ammonia. | |
| WATER (91.5%) | The liquid portion of blood. Acts as a solvent and suspending medium for components of blood; absorbs, transports, and releases heat. | |
| PLASMA PROTEIN (7.0%) | Exert colloid osmotic pressure, which helps maintain water balance between blood and tissues and regulates blood volume. | |
| ALBUMIN | Smallest and most numerous blood plasma proteins; produced by the liver. Transports proteins for several steroid hormones and for fatty acids. | |
| GLOBULINS | Produces by liver and plasma cells, which develop from B lymphocytes. Antibodies help attack viruses and bacteria. Alpha and beta globulins transport iron, lipids, and fat-soluble vitamin. | |
| FIBRINOGEN | Produces by the liver. Plays an essential role in blood clotting | |
SHORT ANSWERS (2M)
1. What is anemia? How it is caused.
Answer: Anaemia is the inability of the blood to carry enough oxygen to meet body needs. Usually, this is because there are low levels of hemoglobin in the blood, but sometimes it is due to the production of faulty hemoglobin.
• Iron deficiency anemia
• Vitamin deficiency anemia
• Anemia of chronic disease
• Aplastic anemia
• Anemias associated with bone marrow disease
• Sickle cell anemia
• Other anemias
2. Write stages of formation of RBC.
Red blood cells are formed in the red bone marrow of bones. Stem cells in the red bone marrow are called hemocytoblasts. They give rise to all of the formed elements in the blood. If a stem cell commits to becoming a cell called a proerythroblast, it will develop into a new red blood cell
3. Write the normal values and life span of the following:
(a)Hb (b) WBC (c) RBC and (d) platelets
Answer:
(a)Hb male: 13.5-17.5 gm/dl and Female: 12.5-15.5 (Life span-120 days)
(b) WBC (Life span- 13 to 20 days)
Granulocytes
• Neutrophils: 40 to 75%
• Eosinophils: 1 to 6%
• Basophils: < 1%
Agranulocytes
• Monocytes: 2 to 10%
• Lymphocytes: 20 to 50%
(c) RBC (Life span-120 days)
Male: 4.5–6.5 million/mm3
Female: 3.8–5.8 million/mm3
(d) Platelets (Life span 8-11 days) 150, 000 to 450,000/ml
4. Mention different types of anaemia.
Answer:
• Iron deficiency anemia
• Vitamin deficiency anemia
• Anemia of chronic disease
• Aplastic anemia
• Anemias associated with bone marrow disease
• Sickle cell anemia
• Other anemias
5. Thrombocytopenia purpura.
Answer: This condition, which usually affects children and young adults, may be triggered by a viral infection such as measles. Antiplatelet antibodies are formed that coat platelet, leading to platelet destruction and their removal from the circulation. A significant feature of this disease is the presence of purpura, which are hemorrhages into the skin ranging in size from pinpoints to large blotches. The severity of the disease varies from mild bleeding into the skin to severe hemorrhage.
6. What is polycythemia? Give its reasons.
Answer: This means an abnormally large number of erythrocytes in the blood. This increases blood viscosity, slows blood flow, and increases the risk of intravascular clotting, ischemia, and infarction.
• This occurs when the erythrocyte count is normal but the blood volume is reduced by fluid loss, e.g. excessive serum exudate from extensive burns.
• Prolonged hypoxia stimulates erythropoiesis and the number of reticulocytes released into the normal volume of blood is increased. This occurs naturally in people living at high altitudes where the oxygen tension in the air is low and the partial pressure of oxygen in the alveoli of the lungs is correspondingly low.
• Heart or lung disease or heavy smoking can also cause polycythemia.
7. Write the functions of WBC?
Answer
| White Blood Cells(WBCs) or Leukocytes | Combat pathogen and other foreign substances that enter the body. |
| Granular Leukocytes
Neutrophiles |
Phagocytosis. Destruction of bacteria with lysozymes, defensins and strong oxidants, such as superoxide anion, hydrogen peroxide, and hypochlorite anion. |
| Eosinophils | Eliminates parasites, such as worms which are too big to be phagocytosed; phagocytes antigen-antibody complexes & combat the effects of histamine in allergic reactions. |
| Basophils | Liberate heparin, histamine and serotonin in allergic reactions that intensify the overall inflammatory response. |
| Agranular Leukocytes
Lymphocytes(T cells, B cells & natural killer cells) |
Medium immune response, including antigen-antibody reactions. B cells develop into plasma cells, which secrete antibodies, T cells attack invading viruses, cancer cells, and transplanted tissue cells. Natural killer calls attach a wide variety of infectious microbes and certain spontaneously arising tumor cells. |
|
Monocytes |
Acts on the hypothalamus, causing the rise in body temperature with microbial infections; stimulates the production of some globulins by the liver; enhances the production of activated T-lymphocytes; Phagocytosis. |
8. Write the functions of plasma proteins.
| PLASMA PROTEIN (7.0%) | Exert colloid osmotic pressure, which helps maintain water balance between blood and tissues and regulates blood volume. |
| ALBUMIN | Smallest and most numerous blood plasma proteins; produces by liver. Transports proteins for several steroid hormones and for fatty acids. |
| GLOBULINS | Produces by liver and plasma cells, which develop from B lymphocytes. Antibodies help attack viruses and bacteria. Alpha and beta globulins transport iron, lipids and fat soluble vitamin. |
| FIBRINOGEN | Produces by liver. Plays essential role in blood clotting. |
9. What is the Rh factor?
Answer: The red blood cell membrane antigen important here is the Rhesus (Rh) antigen or Rhesus factor. About 85% of people have this antigen; they are Rhesus positive (Rh+) and do not, therefore, make anti-Rhesus antibodies. The remaining 15% have no Rhesus antigen (they are Rhesus negative or Rh−). Rh− individuals are capable of making anti-Rhesus antibodies, but are stimulated to do so only in certain circumstances, e.g. in pregnancy, or as the result of an incompatible blood transfusion.
10. What is the difference between plasma and serum?
Answer: Serum is that part of the blood that is similar in composition with plasma but excludes clotting factors of blood. Plasma is considered as the medium of blood in which RBCs, WBC, and other components of blood are suspended. The components of plasma and serum are similar as both contain hormones, glucose, electrolytes, antibodies, antigens, nutrients, and certain other particles except clotting factors which are present only in plasma.
[Plasma – clotting factors = Serum]
11. Compare erythrocytes, leukocytes, and thrombocytes with respect to size, number per mm3, and life span?
(a) Hb male: 13.5-17.5 gm/dl and Female: 12.5-15.5 (Life span-120 days)
(b) WBC (Life span- 13 to 20 days)
Granulocytes
• Neutrophils: 40 to 75%
• Eosinophils: 1 to 6%
• Basophils: < 1%
Agranulocytes
• Monocytes: 2 to 10%
• Lymphocytes: 20 to 50%
(c) RBC (Life span-120 days)
Male: 4.5–6.5 million/mm3
Female: 3.8–5.8 million/mm3
(d) Platelets (Life span 8-11 days) 150, 000 to 450,000/ml
12. What is hemophilia? Describe its signs and symptoms.
Answer: Hemophilia is an inherited deficiency of clotting in which bleeding may occur spontaneously or after only minor trauma. Hemophilia is characterized by spontaneous or traumatic subcutaneous and intramuscular hemorrhaging, nosebleeds, blood in the urine, and hemorrhages in joints that produce pain and tissue damage.
13. Write any four factors hastening the clotting.
Answer:
• I Fibrinogen
• II Prothrombin
• III Tissue factor (thromboplastin)
• IV Calcium (Ca2+)
• V Labile factor, proaccelerin, Ac-globulin
• VII Stable factor, proconvertin
• VIII Antihaemophilic globulin (AHG), antihaemophilic factor A
• IX Christmas factor, plasma thromboplastin component (PTA), antihaemophilic factor B
• X Stuart Prower factor
• XI Plasma thromboplastin antecedent (PTA), antihaemophilic factor C
• XII Hageman factor
• XIII Fibrin stabilizing factor
• Vitamin K is essential for the synthesis of factors II, VII, IX, and X.
Read Also:
Chapter 1. Scope of anatomy and physiology, basic terminologies used in this subject
Chapter 2. Structure of cell – its components and their functions.
Chapter 3. Elementary Tissues of The Human Body
Chapter – 4 . Osseous System Question Answer Bank